Irritable bowel syndrome: a disease of the microbiota?
This article will help you understand what irritable bowel syndrome, or functional colopathy, is. Discover the symptoms of irritable bowel syndrome and the role of microbiota in these symptoms: you will learn how to diagnose intestinal dysbiosis in cases of irritable bowel syndrome. We will also explain what the FODMAP diet is and what foods reduce the symptoms of this syndrome.
What is irritable bowel syndrome or functional colopathy?
Irritable bowel syndrome (IBS), also known as functional bowel disorder or irritable bowel syndrome, affects 10 to 15% of the world's population, two-thirds of whom are women. It is a multifactorial disease involving genetic and environmental factors (stress, diet, age, geographical origin, antibiotic treatment, infections, etc.). This disease is the main reason for gastroenterology consultations, accounting for up to half of them!

What are the symptoms of irritable bowel syndrome?
Irritable bowel syndrome is characterized by chronic abdominal pain, bloating, and digestive problems, often associated with fatigue, anxiety, or depression (up to 75% of patients), nausea, headaches, and sleep disorders. This condition is considered benign because it does not develop into cancer (e.g., colorectal cancer). It is also called functional bowel disorder because it does not cause structural changes in the intestine.
Is it difficult to diagnose irritable bowel syndrome?
Patients sometimes have to overcome a real obstacle course to get a diagnosis of irritable bowel syndrome. Diagnosis often takes a long time (from several months to several years), as the symptoms can be associated with other diseases such as chronic inflammatory bowel disease or gluten allergy.
Patients often hear that stress is the source of their problems. This lack of understanding, along with the wide range of symptoms, impacts their quality of life and mental and social well-being. Pain and discomfort lead patients to decline dinner invitations and eat alone to avoid questions from those around them. They may feel guilty, believing that stress is responsible for their problems. In addition, intestinal disorders are a taboo subject that people rarely dare to discuss with their loved ones.
The diagnosis of this disease is based on the Rome criteria. The patient must have experienced recurrent abdominal pain at least once a week for at least the previous three months, with symptoms appearing more than six months ago. This pain must be associated with transit disorders. Functional colopathy can be associated with constipation or diarrhea.
It should be noted that women suffer from IBS associated with constipation more often than men. As these signs can also be observed in other diseases, the practitioner must proceed by process of elimination through questioning and additional tests.
The causes of abdominal pain are motility disorders (progression of stool through the intestine), intestinal hypersensitivity, immune activation, intestinal microbiota imbalance, and intestinal barrier disturbances.
At present, there is no cure for IBS. The available drug and probiotic treatments can relieve certain symptoms but do not cure the disease.
Is the microbiota the cause of irritable bowel syndrome?
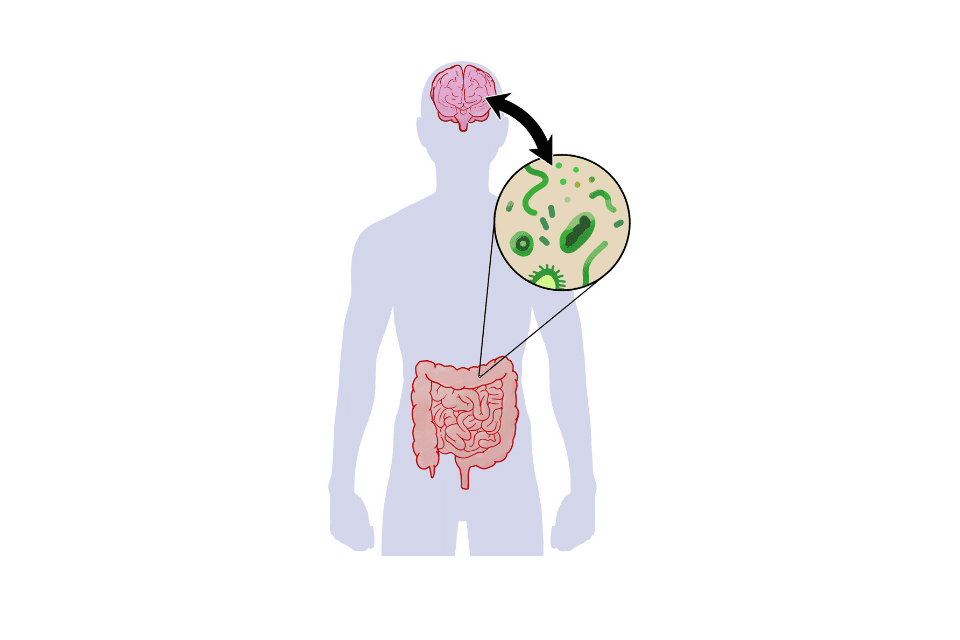
The gut microbiota, the collection of microorganisms that colonize the intestine, plays a major role in perpetuating symptoms. The gut-brain axis is a bidirectional system that integrates the brain and gastrointestinal functions such as motility, appetite, and weight maintenance, and in which the gut flora plays a key role. In addition, the loss of microbiota balance, known as dysbiosis, is thought to play a role in initiating IBS and contributing to symptoms. This dysbiosis is characterized by an increase in pathogenic species and a decrease in lactobacilli and bifidobacteria.
It triggers an immune response and low-grade inflammation, which is why irritable bowel syndrome is now thought to be a disease of the microbiota and the gut-brain axis. A loss of bacterial diversity has been measured in more than 70% of cases. These abnormalities in the microbiota and the consequences on the gut-brain axis lead to changes in intestinal motility and secretions, contributing to visceral hypersensitivity and alterations in the enterocrine (hormone production) and immune systems.
IBS frequently occurs following a severe intestinal infection, or gastroenteritis, which has reduced the diversity of the intestinal flora and is often accompanied by SIBO (small intestinal bacterial overgrowth). Antibiotic treatments and stress are also risk factors, as are genetic susceptibilities.
Take care of your microbiota with Nahibu.
Is irritable bowel syndrome an inflammatory disease?
A 15 to 50% increase in intestinal permeability has been measured in patients. This hyperpermeability allows the microbiota to cause inflammation and could affect the central nervous system by increasing the level of cytokines (inflammatory molecules) infiltrating the circulation. The low-level inflammation thus created causes visceral hypersensitivity to pain, neuromuscular dysfunction, and transit disorders in cases of irritable bowel syndrome.
The infiltration of immune cells near visceral neurons observed in some patients is associated with bloating, pain, and symptom severity.
Stress is an aggravating factor in IBS because it activates the immune system.

What to eat if you have irritable bowel syndrome?
Irritable bowel syndrome is more common in Western societies, suggesting that diet plays a role in IBS, as we know that a Western diet (high in fast-acting sugars, saturated fats, and processed foods) causes the development of pro-inflammatory microbiota.
In addition, up to 89% of patients experience symptoms triggered by meals and the ingestion of specific foods. It is in this context that research began on FODMAPs, fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These sugars are poorly digested by our bodies but are rapidly fermented by our gut bacteria.

Why are FODMAPs bad for IBS patients?
The compounds produced mainly during the fermentation of FODMAPs are short-chain fatty acids (SCFAs), which are beneficial to health. However, in IBS patients, some of the microbes that produce SCFAs are altered, and consuming FODMAPs increases gas volume and abdominal pain. Patients with increased visceral sensitivity experience even more painful bloating and gas. Does this mean we should stop eating FODMAPs? No, in people who do not suffer from irritable bowel syndrome, FODMAPs do not cause any problems and can be consumed without restriction.
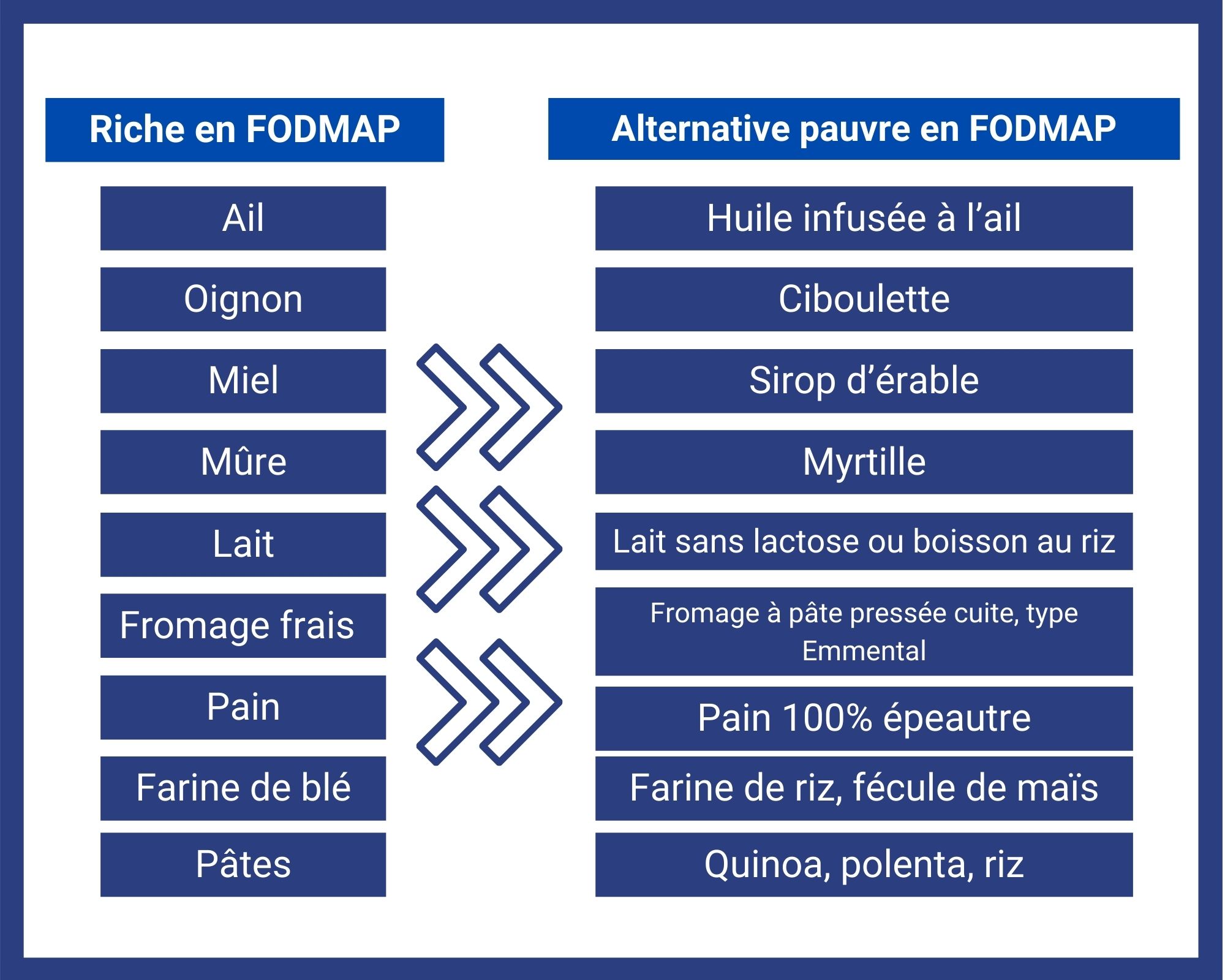
A reduction in the severity of symptoms (bloating, diarrhea, and pain) and an improvement in quality of life are observed in approximately 70% of patients following a low-FODMAP diet. These compounds are found in a wide variety of foods (Photo [Shido*]), such as certain fruits and vegetables, grains, dairy products, and processed foods, so it is difficult to eliminate them from your diet. In addition, a low-FODMAP diet should not be maintained for more than a few months. The implementation of such a diet must be supervised by a dietitian, otherwise it may be ineffective and lead to weight loss, deficiencies, or imbalances.
It should be noted that one study showed that the improvement in pain achieved through a low-FODMAP diet was not accompanied by an improvement in constipation or diarrhea.
What is the low-FODMAP diet?
To relieve symptoms and identify the sugars and foods that patients are intolerant to, they can follow a low-FODMAP diet for 4 to 8 weeks; this is the elimination phase, which aims to give the gut a rest. Following this phase, foods containing FODMAPs (see our low-FODMAP recipes) are reintroduced one by one on a daily basis to test tolerance. This allows patients to identify the foods that cause them symptoms and that they should therefore avoid. Conversely, foods that do not cause symptoms can be kept in the patient's diet.
Recipes for the irritable bowel syndrome diet
To relieve pain, bloating, and other symptoms of irritable bowel syndrome, many patients turn to the low-FODMAP diet. At Nahibu, we offer low-FODMAP recipes to support you during the elimination phase. The term low-FODMAP is indicated in the recipe text. To help you in your kitchen, here is also a list of alternatives to high-FODMAP foods. Replace high-FODMAP foods with alternatives that contain little or no FODMAPs.
Can IBS be treated with probiotics?
Probiotics are live microorganisms that, when administered in adequate amounts, have a positive effect on the host. Learn more about probiotics and prebiotics. The combination of lactobacilli and bifidobacteria helps restore the integrity of the intestinal barrier. It is now accepted that regular intake of certain probiotics relieves the symptoms of irritable bowel syndrome.
Studies have shown that in IBS patients with constipation, transit disorders and abdominal distension improve after one month of taking Bifidobacterium lactis. After two months of taking Bifidobacterium infantis, the production of certain inflammatory molecules is normalized and symptoms are improved.
How to live well with irritable bowel syndrome?
Irritable bowel syndrome is a multifactorial condition that is difficult to diagnose and often leaves patients wandering from doctor to doctor and suffering for several years. In addition to physical symptoms, psychological consequences are also observed in patients.
First and foremost, listen to your body: suffering from chronic pain or abdominal distension for several months or even years is not normal. What should you do if you experience these symptoms and think you may have IBS? Consult a doctor who can listen to you and refer you to a specialist if necessary.
Analysis of the intestinal flora to detect dysbiosis.
You can have your gut microbiota analyzed to detect dysbiosis, or an imbalance in your gut flora. The microbiota plays a major role in functional bowel disorders.
Once the diagnosis has been confirmed by a doctor, the question you will ask yourself is what should I eat if I have irritable bowel syndrome? If you want to test your tolerance to certain FODMAPs, you can exclude them for several weeks, with the help of a dietitian, to see if this relieves your symptoms. Then reintroduce the excluded foods one by one to test your tolerance. Seek the support of a dietitian who will motivate you and ensure that you do not suffer from any deficiencies. You will then know which foods to avoid in order to reduce pain, bloating, gas, and other discomforts.
Don't blame yourself. Stress is not the source of all your problems if you suffer from irritable bowel syndrome. However, it is an aggravating factor. It is therefore recommended that you adopt relaxation techniques such as meditation, cardiac coherence, or yoga to prevent your symptoms from worsening.
Finally, don't be afraid to talk about it. A large part of the population suffers from this increasingly well-known condition, so you are not alone. Don't hesitate to explain your symptoms so that those around you understand what you are going through and can support you as best they can, especially at mealtimes. You may also feel a weight lifted off your shoulders!
Sources:
Irritable Bowel Syndrome: Epidemiology, Pathophysiology, Diagnosis, and Treatment. Dean Nathanial Defrees and Justin Bailey, 2017
Irritable bowel syndrome, the microbiota and the gut-brain axis. Hans Raskov, Jakob Burcharth, Hans-Christian Pommergaard and Jacob Rosenberg, 2016
Pathophysiology of irritable bowel syndrome. Gerald J Holtmann, Alexander C Ford and Nicholas J Talley, 2016

Discover more articles on the microbiota.
Is an unbalanced microbiota the cause of obesity?
According to the WHO, 41 million children under the age of 5 were overweight or obese in 2016. It is said that an "obesogenic" microbiota develops from birth. So what role does the microbiota play in obesity?
What are inflammatory bowel diseases?
Chronic inflammatory bowel diseases affect 250,000 people in France and are characterized by inflammation of the digestive tract.
Does the gut microbiota play a role in colorectal cancer?
Colorectal cancer, colon cancer? We explain everything you need to know about symptoms, risk factors, diet, and how gut microbiota plays a role in this disease.
Take care of your microbiota with Nahibu.